Effect of low level laser on dental pulp tissue during orthodontic movement
Keywords:
Laser, Low level laser, dental pulp, ortodonthic tratmentMain Article Content
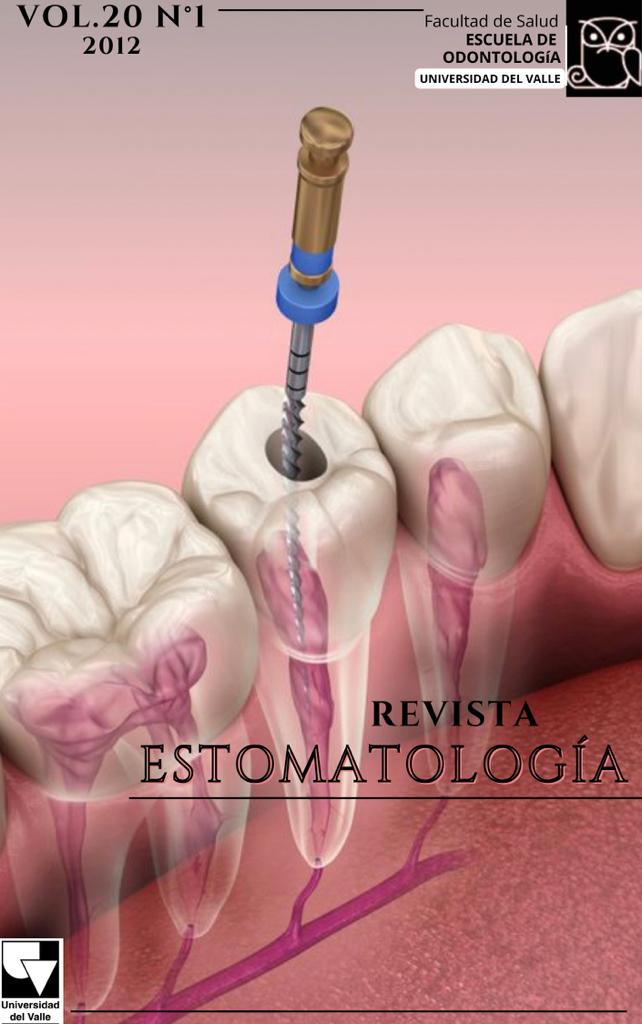
Low level laser application in orthodontics attempts to accelerate the induced orthodontic movement and to dissipate the dental discomfort during treatment. The recognition of its biological foundation is a fundamental issue to understand the effect of all tissues involved in the irradiated zone. There have been research findings on the cell proliferation and empowerment of cell functions, promotion of bone remodeling, and decreasing of the local swelling and pain during orthodontic treatments. However, the positive results of the laser application on cells involved in the orthodontic movement have not widely been investigated. Literature indicates a lack of research finding on the effect of low laser therapy on the dentin-pulp complex, which demands randomized controlled trials. For these reasons, the aim of this paper attempts to compile the main publications done regarding the effect of low level laser therapy on dental pulp tissue.
2. Scott P, Sherriff M, DiBiase AT, Cobourne MT. Perception of discomfort during initial orthodontic tooth alignment using a self-ligating or conventional bracket system: a randomized clinical trial. Eur J Orthod. 2008; 30:227-232.
3. Fleming P, Johal A. Self-Ligating Brackets in Orthodontics, A Systematic Review. Angle Orthod. 2010; 80:575-584.
4. Turhani D, Scheriau M, Kapral D, Benesch T, Jonke E, Bantleon HP. Pain relief by single low-level laser irradiation in orthodontic patients undergoing fixed appliance therapy. Am J Orthod Dentofacial Orthop. 2006; 130:371-7.
5. Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M. Th effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci. 2008; 23(1):27-33.
6. Tortamano A, Lenzi D, Haddad A, Bottino M, Dominguez G, Vigorito J. Low-level laser therapy for pain caused by placement of the first orthodontic archwire: A randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics.2009; 136(5):662-7.
7. Lacerda M, Amadei R, Arizawa E. The effect of two phototherapy protocols on pain control in orthodontic procedure a preliminary clinical study. Lasers Med Sci. 2011; 26(5):657-63.
8. Rodríguez C, Vanín D, Efectos de Ortodoncia en la Pulpa Dental. Revista Estomatología 2006; 14(1):27-2.
9. Cohen S, Burns R. Vías de la Pulpa. Octava Edición. Elsevier Science. Madrid España 2002.
10. Uzel A, Buyukyilmaz T, Kayalioglu M, Uzel I. Temperature rise during orthodontic bonding with various light-curing units-an in vitro study. Angle Orthod. 2006; 76(2):330-4.
11. Ulusoy C, Irmak O, Bagis YH, Ulusoy OI. Temperature rise and shear bond strength of bondable buccal tubes bonded by various light sources. Eur J Orthod. 2008; 30(4):413-7
12. Malkoç S, Uysal T, Usümez S, Isman E, Baysal A. In-vitro assessment of temperature Rise in the pulp during orthodontic bonding. Am J Orthod Dentofacial
Orthop. 2010; 137(3):379-83
13. Uysal T, Eldeniz AU, Usumez S, Usumez A. Thermal changes in the pulp chamber during different adhesive clean up procedures. Angle Orthod. 2005; 75(2):220-5.
14. Jonke E, Weiland F, Freudenthaler J, Bantleon H. Heat Generated Adhesive Removal After Debonding of Brackets by Residual adhesive. World Journal of Orthodontics 2006; 7(4): 357-360.
15. Hamersky PA, Weimer AD, Taintor JF. The effect of orthodontic force application on the pulpal tissue respiration rate in the human premolar. Am J Orthod. 1980 Apr; 77(4):368-78.
16. Kim S. Neurovascular interactions in the dental pulp in health and inflammation. J Endod 16:48-53, 1990.
17. Kim S, Dorsher-Kim J: Hemodynamic regulation of the dental pulp in a low compliance environment. J Endod 1989; 15:404-408.
18. Hamilton, R, Gutman, J.L. Endodontic-Orthodontic relationships: a review of integrated treatment planning challenges. Int. Endod. Journal. 1999; 32:343-60
19. Babacana H, Doruka C, Bicakci A. Pulpal blood flow changes due to rapid maxillary expansion. The Angle Orthodontist: 2010,;80 (6): 1136-1140.
20. Perinetti G, Varvara G, Salini L, Tet S.Alkaline phosphatase activity in dental pulp of orthodontically treated teeth. American Journal of Orthodontics and Dentofacial Orthopedics2005; 128(4):492-6.
21. Perinetti G, Varvara G, Festa F, Esposito P. Aspartate aminotransferase activity in pulp of orthodontically treated teeth. Am J Orthod Dentofacial Orthop. 2004; 125(1):88-92.
22. Barwick P.J, Ramsay D.S, Effect of brief intrusive force on human pulpal blood flow. Am J Orthod Dentofac Orthop 1996; 110:273-9.
23. Ikawa M, Fujiwara M, Horiuchi H, Shimauchi H. The effect of short-term tooth intrusion on human pulpal blood flow measured by laser Doppler flowmetry. Arch Oral Biol. 2001; 46(9):781-787
24. Sano Y, Ikawa M, Sugawara J, Horiuchi H, Mitani H. The effect of continuos intrusive force on human pulpal blood flow. Eur J Orthod. 2002; 24:159-16
25. Villa P, Oberti G, Moncada C, Vasseur O, Jaramillo A, Tobón D, et al. Pulp-dentine complex changes and root resorption during intrusive orthodontic tooth movement in patients prescribed nabumetone. Journal of Endodontics2005; 31(1):61-6.
26. Mostafa Y.A., Iskander K.G., El-Mangoury N.H. Iatrogenic pulpal reactions to orthodontic extrusion. Am J Orthod Dentofac Orthop 1991; 99:30-4
27. Sübay, R.K., Kaya H., Tarim B., Sübay A., Cox C.F., Response of human pulpal tissue to orthodontic extrusive applications. Journal of Endodontics. 2001; 27(8): 508-511.
28. Masaru Y, Kazutaka K. The Effects of Orthodontic Mechanics on the Dental Pulp. Semin Orthod 2007; 13:272-280.
29. Derringer KA, Jaggers DC, Linden RW: Angiogenesis in human dental pulp following orthodontic tooth movement. J Dent Res.1996; 75:1761-1766.
30. Derringer KA, Linden RW: Vascular endothelial growth factor, fibroblast growth factor 2, platelet derived growth factor and transforming growth factor beta released in human dental pulp following orthodontic force. Arch Oral Biol.2004; 49:631-641.
31. Parris WG, Tanzer FS, Fridland GH, et al: Effects of orthodontic force on methionine enkephalin and substance P concentrations in human pulpal tissue. Am J Orthod Dentofacial Orthop.1989; 95:479-489.
32. Tuncer LI, Alaçam T, Oral B. Substance P expression is elevated in inflamed human periradicular tissue. J Endod 2004; 30: 329-332.
33. Yamaguchi M, Kojima T, Kanekawa M, et al: Neuropeptides stimulate production of interleukin-1 beta, interleukin- 6, and tumor necrosis factor-alpha in human dental pulp cells. Inflamm Res.2004; 5:199-204.
34. Yamaguchi M, Ozawa Y, Mishima H, Aihara N, Kojima T, Kasai K. Substance P increases production of proinflammatory cytokines and formation of osteoclasts in dental pulp fibroblasts inpatients with severe orthodontic root resorption. Am J Orthod Dentofacial Orthop. 2008; 133(5):690-8.
35. Walker JA, Tanzer FS, Harris EF, Wakelyn C, Desiderio DM. The enkephalin response in human tooth pulp to orthodontic force. Am J Orthod Dentofac Orthop 1987; 92:9-16.
36. Parris WG, Tanzer FS, Fridland GH, Harris EF, Killmar J, Desiderio DM. Effects of forcé on methionine enkephalin and substance P concentrations in human pulpal tissue. Am J Orthod Dentofac Orthop 1989; 95:479-489.
37. Awawdeh L, Lundy FT, Shaw C, Lamey PJ, Linden GJ, Kennedy JG. Quantitative analysis of substance P, neurokinin A and calcitonin gene-related peptide in pulp tissue from painful and healthy human teeth. Int Endod J. 2002; 35(1):30-6.
38. Butcher EO, Taylor AC. The vascularity of the incisor pulp of the monkey and its alteration by tooth retraction. J Dent Res 1952; 31:239-247.
39. Anstendig HS, Kronman JH. A histological study of pulpal reaction to orthodontic tooth movement in dogs. Angle Orthod 1972; 42:50-55.
40. Turley PK, Joiner MW, Hellstrom S: The effect of orthodontic extrusion on traumatically intruded teeth. Am J Orthod 85:47-56, 1984
41. Kvinnsland S, Heyeraas K, Ofjord ES. Effect of experimental tooth movement on periodontal and pulpal blood flow. Eur J Orthod. 1989; 11(3):200-5.
42. Norevall LI, Forsgren S, Matsson L: Expression of neuropeptides (CGRP, substance P) during and after orthodontic tooth movement in the rat. Eur J Orthod 1995; 17:311-325.
43. Vandevska-Radunovic V, Kvinnsland S, Kvinnsland I. Effect of experimental tooth movement on nerve fibres immunoreactive to calcitonin gene-related peptide, protein gene product 9.5, and blood vessel density and distribution in rats. Eur J Orthod. 1997; 19:517-529.
44. Santamaria Jr. M, Milagres D, Iyomasa M, Stuani M, Ruellas A. Initial pulp changes during orthodontic movement: histomorphological evaluation. Brazilian Dental Journal.2007; 18:34-9.
45. Lim H, Lew K, Tay D. A clinical investigation of the efficacy of low level laser therapy in reducing orthodontic post adjustment pain. American Journal of Orthodontics and Dentofacial Orthopedics1995; 108(6):614-22.
46. Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012; 40(2):516-33.
47. Sroka R, Schaffer M, Fuchs C, Pongratz T, Schrader-Reichard U, Busch M, Schaffer PM, Dühmke E, Baumgartner R. Effects on the mitosis of normal and tumor cells induced by light treatment of different wavelengths. Lasers Surg Med.1999; 25:263-71.
48. Zhang J, Xing D, Gao X. Low-power laser irradiation activates Src tyrosine kinase through reactive oxygen species-mediated signaling pathway. J Cell Physiol. 2008; 217:518-28.
49. Miyata H, Genma T, Ohshima M, Yamaguchi Y, Hayashi M, Takeichi O, Ogiso B, Otsuka K. Mitogen-activated protein kinase/extracellular signal-regulated protein kinase activation of cultured human dental pulp cells by low-power gallium-aluminium-arsenic laser irradiation. Int Endod J.2006; 39:238-44.
50. Gao X, Chen T, Xing D, Wang F, Pei Y, Wei X. Single cell analysis of PKC activation during proliferation and apoptosis induced by laser irradiation. J. Cell. Physiol. 2006; 206:441-8.
51. Kujawa J, Zavodnik L, Zavodnik I, Buko V, Lapshyna A, Bryszewska M. Effect of low-intensity (3.75-25 J/cm2) nearinfrared (810 nm) laser radiation on red blood cell ATPase activities and membrane structure. J Clin Laser Med Surg. 2004; 22:111-7.
52. Kujawa J, Zavodnik L, Zavodnik I, Bryszewska M. Low intensity near-infrared laser radiation-induced changes of acetylcholinesterase activity of human erythrocytes. J Clin Laser Med Surg. 2003; 21:351-5.
53. Kujawa J, Zavodnik IB, Lapshina A, Labieniec M, Bryszewska M. Cell survival, DNA, and protein damage in B14 cells under low-intensity near-infrared (810 nm) laser irradiation. Photomed Laser Surg. 2004; 22:504-8.
54. Lirani-Galvão, A. P., V. Jorgetti, and O. L. Silva. Comparative study of low-level laser therapy and low-intensity pulsed ultrasound effect on bone in rats. Photomed Laser Surg 2006. 24:735–740.
55. Coluzzi, D. J. An overview of laser wavelengths used in Dentistry. Dent Clin N Am. 2000; 44:753-765.
56. Demir H, Yaray S, Kirnap M, Yaray K. Comparison of the effects of laser and ultrasound treatments on experimental wound healing in rats. J Rehabil Res Dev. 2004.41:721-728.
57. Koichiro, K. and N. Shimizu. Effect of low-energy laser irradiation on bone remodeling during experimental tooth movement in rats. Laser Surg Med 2000. 26:282–291.
58. Ueda, Y. and N. Shimizu. Effects of pulse frequency of low-level laser therapy (LLLT) on bone nodule formation in rat calvarial cells. J Clin Laser Med Surg 2003. 21:271–277.
59. Eduardo C, de Freitas P, Esteves-Oliveira M, Aranha a, Müller K, Simões a, Bello M, Turner J. Laser phototherapy in the treatment of periodontal disease. A review. Lasers Med Sci .2010; 25:781–792.
60. Lopes, Almeida. Comparison of the low level laser therapy effects on cultured human gingival fibroblasts proliferation using different irradiance and same fluence. Lasers Surg ed. 2001; 29(2):179-84
61. Pereira AN. Effect of low-power laser irradiation on cell growth and procollagen synthesis of cultured fibroblasts. Lasers Surg Med.2002: 31(4):263-7.
62. Kreisler M. Effect of low-level GaAlAs laser irradiation on the proliferation of human periodontal ligament fibroblasts: an in vitro study. J Clin Peridontol. 2003: 30(4):353-8.
63. Choi EJ, Yim JY, Koo KT, Seol YJ, Lee YM, Ku Y, Rhyu IC, Chung CP, Kim TI. Biological effects of a semiconductor diode laser on human periodontal ligament fibroblasts. J Periodontal Implant Sci. 2010; 40(3):105-10.
64. Saygun I, Karacay S, Serdar M, Ural AU .Effects of laser irradiation on the release of basic fibroblast growth factor (bFGF), insulin like growth factor-1 (IGF-1), and receptor of IGF-1(IGFBP3) from gingival fibroblasts. Lasers Med Sci. 2008; 23(2):211-5.
65. Domínguez A, Clarkson A, López R. An in vitro study of the reaction of periodontal and gingival fibroblasts to low- level laser irradiation: A pilot study. J Oral Laser Applications. 2008; 8:235-244.
66. Dominguez A, Castro P, Morales M. An In Vitro Study of the Reaction of Human
Osteoblasts to Low-level Laser Irradiation. Journal of Oral Laser Applications. 2009; 9(1):21-28
67. Domínguez A, Morales M, Zúñiga P. Cellular Effects related to the clinical uses of laser in orthodontics. Journal of Oral Laser Applications.2009; 9:199-203.
68. Coombe AR, Darendeliler N. The effects of low level laser irradiation on osteoblastic cells. Clin Orthod Res. 2001; 4:3-14.
69. Fujihara NA, Hiraki KR, Marques MM. Irradiation at 780nm increases proliferation rate of osteoblasts independently of dexamethasone presence. Lasers Surg Med. 2006; 38:332-336
70. Ozawa Y, Shimizu N, Kariya G, Abiko Y. Low-energy laser irradiation stimulates bone nodule formation at early stages of cell culture in rat calvarial cells. Bone 1998; 22:347-354.
71. Masoud S, Abbasnia E, Fathi M, Sahraei S. The effects of low-level laser irradiation on differentiation and proliferation of human bone marrow mesenchymal stem cells into neurons and osteoblasts an in vitro study. Lasers Med Sci. Published online May 20 2011.
72. Saito S, Shimizu N. Stimulatory effects of low-power laser irradiation on bone regeneration in midpalatal suture during expansion in the rat. Am J Orthod Dentofacial Orthop. 1997; 111 (5):525-32.
73. Kawasaki K, Shimizu N. Effects of low-energy laser irradiation on bone remodeling during experimental tooth movement in rats. Lasers Surg Med. 2000; 26(3):282-91.
74. Habib FA, Gama SK, Ramalho LM, Cangussú MC, Santos Neto FP, Lacerda JA, Araújo TM, Pinheiro AL. Laser-induced alveolar bone changes during orthodontic movement: a histological study on rodents. Photomed Laser Surg. 2010; 28(6):823-30.
75. Aihara N, Yamaguchi M, Kasai K. Low–energy irradiation stimulates formation of osteoclast-like cells via RANK expression in Vitro. Lasers Med Sci. 2006; 21(1): 24-33.
76. Fujita S, Yamaguchi M, Utsunomiya T, Yamamoto H, Kasai K. Low-energy laser stimulates tooth movement velocity via expression of RANK and RANKL. Orthod Craniofac Res. 2008; 11(3):143-55.
77. Yamaguchi M, Hayashi M, Fujita S, Yoshida T, Utsunomiya T, Yamamoto H, et al. Low energy laser irradiation facilitates the velocity of tooth movement and the expressions of matrix metalloproteinase-9, cathepsin K, and alpha (v) beta (3) integrin in rats. The European Journal of Orthodontics. Eur J Orthod. 2010; 32(2):131-9.
78. Abello M, Valbuena D. Efecto del Laser blando en la velocidad de alineación del movimiento ortodóncico. Tesis de Postgrado Fundación CIEO Bogotá Colombia1996.
79. Cruz D, Kohara E, Ribeiro M, Wetter N. Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: a preliminary study. Lasers in surgery and medicine. 2004; 35(2):117-20.
80. Limpanichkul W, Godfrey K, Srisuk N, Rattanayatikul C. Effects of low-level laser therapy on the rate of orthodontic tooth movement. Orthodontics and Craniofacial Research. 2006; 9(1):38-43.
81. Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M. The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci. 2008; 23(1):27-33
82. Dominguez A., Velasquez S. (2010) Acceleration effect of orthodontic movement by application of low-intensity laser. J Oral .Laser Applications. 2010 (10): 99-105.
83. Sousa MV, Scanavini MA, Sannomiya EK,Velasco LG, Angelieri F. Influence of low-level laser on the speed of orthodontic movement. Photomed Laser Surg. 2011; 29(3):191-6.
84. Blechman A. Pain-free and mobility-free orthodontics? American Journal of Orthodontics and Dentofacial Orthopedics1998; 113(4):379-83.
85. Otasevic M, Naini F, Gill D, Lee R. Prospective randomized clinical trial comparing the effects of a masticatory bite wafer and avoidance of hard food on pain associated with initial orthodontic tooth movement. American Journal of Orthodontics and Dentofacial Orthopedics. 2006; 130(1):6.
86. O’Connor PJ. Patients’ perceptions before, during, and after orthodontic treatment. Journal of Clinical Orthodontics. 2000; 34:591-592.
87. Ngan P, Kess B, Wilson S. Perception of discomfort by patients undergoing orthodontic treatment. American Journal of Orthodontics and Dentofacial Orthopedics. 1989; 96:47-53.
88. Brown DF, Moerenhout RG. The pain experience and psychological adjustments to orthodontic treatment of preadolescents, adolescents and adults. American Journal of Orthodontics and Dentofacial Orthopedics 1991; 100:349-356.
89. Scheurer PA, Firestone AR, Bürgin WB. Perception of pain as a result of orthodontic treatment with fixed appliances. European Journal of Orthodontics. 1996; 18:349-357.
90. Firestone AR, Scheurer PA, Bürgin WB. Patient’s anticipation of pain and pain-related side effects, and their perception of pain as a result of orthodontic treatment with fixed appliances. European Journal of Orthodontics. 1999; 21:387-396.
91. Bergius M, Kiliardis S, Berggren U. Pain in orthodontics a review and discussion of the literature. Journal of Orofacial Orthopedics. 2000; 61:125-137.
92. Polat O, Karaman AI. Pain control during fixed orthodontic appliance Therapy. Angle Orthod. 2005; 75:214-219.
93. Salmassian R, Oesterle L, Shellhart W, Newman S. Comparison of the efficacy of ibuprofen and acetaminophen in controlling pain after orthodontic tooth movement. American Journal of Orthodontics and Dentofacial Orthopedics 2009; 135(4):516-21
94. Ngan PW, Hägg U, Yin C .The effect of ibuprofen on the level of discomfort in patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1994; 106:88-95
95. Law SLS, Southard KS, Law AS, Logan HL, Jakobsen JR. An evaluation of postoperative ibuprofen treatment of pain associated with orthodontic separator placement. Am J Orthod Dentofacial Orthop.2000; 118:629-635
96. Arias O, Marquez-Orozco M. Aspirin, acetaminophen, and ibuprofen: their effects on orthodontic tooth movement. American Journal of Orthodontics and Dentofacial Orthopedics.2006; 130(3):364-70.
97. Lim HM, Lew KK, Tay DK. A clinical investigation of the low level laser therapy in reducing orthodontic postadjustment pain. Am J Orthod Dentofacial Orthop.1995; 108:614-622.
98. Harazaki M, Takahashi H, Ito A, Isshiki Y (1998) Soft laser irradiation induced pain reduction in orthodontic treatment. Bull Tokyo Dent Coll.1998; 39:95.101.
99. Tortamano a, Lenzi D, Haddad a, Bottino M, Dominguez G, Vigorito J. Low-level laser therapy for pain caused by placement of the first orthodontic archwire: A randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics. 2009; 136(5):662-7.
100. Xiaoting L, Yin T, Yangxi C. Interventions for pain during fixed orthodontic appliance therapy. A systematic review. Angle Orthod. 2010; 80(5):925-32.
101. Abi-Ramia L, Stuani A, Stuani M, de Moraes Mendes A. Effects of Low-Level Laser Therapy and Orthodontic Tooth Movement on Dental Pulps in Rats. Journal Information. Angle Orthod. 2010; 80(1):116-22.
102. de Alencar Mollo M, Frigo L, Favero GM, Lopes-Martins RA, Brugnera Junior A. In vitro analysis of human tooth pulp chamber temperature after low-intensity laser herapy at different power outputs. Lasers Med Sci. 2011; 26(2):143-7.
Downloads
Los autores/as conservan los derechos de autor y ceden a la revista el derecho de la primera publicación, con el trabajo registrado con la licencia de atribución de Creative Commons, que permite a terceros utilizar lo publicado siempre que mencionen la autoría del trabajo y a la primera publicación en esta revista.